Hip Bursitis-OrthoInfo - AAOS - Dr Ronak Patel MD
Physical therapy. Your doctor may prescribe exercises to increase hip strength and flexibility. You may do these exercises on your own, or a physical therapist
adsPart of the document
Hip Bursitis
This article is also available in Spanish: Bursitis de cadera (Hip Bursitis) (topic.cfm?topic=A00724).
Bursae, are small, jelly-like sacs that are located throughout the body, including around the shoulder, elbow, hip,
knee, and heel. They contain a small amount of fluid, and are positioned between bones and soft tissues, acting as
cushions to help reduce friction.
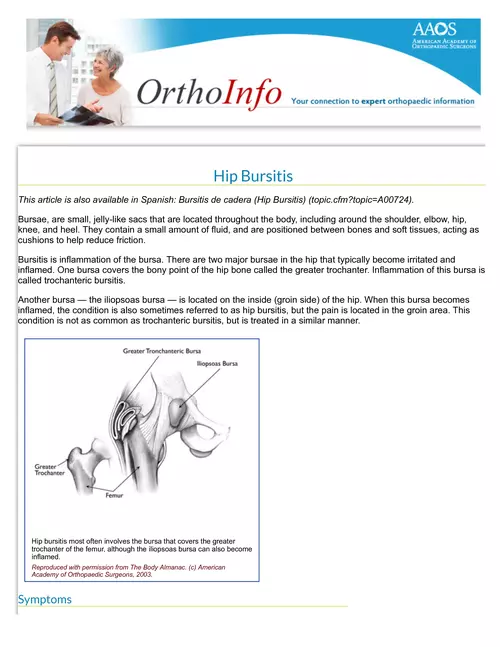
Bursitis is inflammation of the bursa. There are two major bursae in the hip that typically become irritated and
inflamed. One bursa covers the bony point of the hip bone called the greater trochanter. Inflammation of this bursa is
called trochanteric bursitis.
Another bursa - the iliopsoas bursa - is located on the inside (groin side) of the hip. When this bursa becomes
inflamed, the condition is also sometimes referred to as hip bursitis, but the pain is located in the groin area. This
condition is not as common as trochanteric bursitis, but is treated in a similar manner.
Hip bursitis most often involves the bursa that covers the greater
trochanter of the femur, although the iliopsoas bursa can also become
inflamed.
Reproduced with permission from The Body Almanac. (c) American
Academy of Orthopaedic Surgeons, 2003.
Symptoms
The main symptom of trochanteric bursitis is pain at the point of the hip. The pain usually extends to the outside of
the thigh area. In the early stages, the pain is usually described as sharp and intense. Later, the pain may become
more of an ache and spread across a larger area of the hip.
Typically, the pain is worse at night, when lying on the affected hip, and when getting up from a chair after being
seated for a while. It also may get worse with prolonged walking, stair climbing, or squatting.
Risk Factors
Hip bursitis can affect anyone, but is more common in women and middle-aged or elderly people. It is less common
in younger people and in men.
The following risk factors have been associated with the development of hip bursitis.
Repetitive stress (overuse) injury. This can occur when running, stair climbing, bicycling, or standing for
long periods of time.
Hip injury. An injury to the point of your hip can occur when you fall onto your hip, bump your hip, or lie on one
side of your body for an extended period of time.
Spine disease. This includes scoliosis, arthritis of the lumbar (lower) spine, and other spine problems.
Leg-length inequality. When one leg is significantly shorter than the other, it affects the way you walk, and
can lead to irritation of a hip bursa.
Rheumatoid arthritis. This makes the bursa more likely to become inflamed.
Previous surgery. Surgery around the hip or prosthetic implants in the hip can irritate the bursa and cause
bursitis.
Bone spurs or calcium deposits. These can develop within the tendons that attach muscles to the
trochanter. They can irritate the bursa and cause inflammation.
Doctor Examination
To diagnose hip bursitis, the doctor will perform a comprehensive physical examination, looking for tenderness in the
area of the point of the hip. He or she may also perform additional tests to rule out other possible injuries or
conditions. These tests can include imaging studies, such as x-rays, bone scanning, and magnetic resonance
imaging (MRI).
Treatment
Nonsurgical Treatment
The initial treatment for hip bursitis does not involve surgery. Many people with hip bursitis can experience
relief with simple lifestyle changes, including:
Activity modification. Avoid the activities that worsen symptoms.
Non-steroidal anti-inflammatory drugs (NSAIDs). Ibuprofen, naproxen, piroxicam, celecoxib, and others,
may relieve pain and control inflammation.Use NSAIDs cautiously and for limited periods. Talk with your
doctor about the NSAIDs you use. NSAIDs may have adverse side effects if you have certain medical
conditions or take certain medications.
Assistive devices. Use of a walking cane or crutches for a week or more when needed.
Physical therapy. Your doctor may prescribe exercises to increase hip strength and flexibility. You may
do these exercises on your own, or a physical therapist may teach you how to stretch your hip muscles
and use other treatments such as rolling therapy (massage), ice, heat, or ultrasound.
Steroid injection. Injection of a corticosteroid along with a local anesthetic may also be helpful in
relieving symptoms of hip bursitis. This is a simple and effective treatment that can be done in the
doctor's office. It involves a single injection into the bursa. The injection may provide temporary
(months) or permanent relief. If pain and inflammation return, another injection or two, given a few
months apart, may be needed. It is important to limit the number of injections, as prolonged
corticosteroid injections may damage the surrounding tissues.
Surgical Treatment
Surgery is rarely needed for hip bursitis. If the bursa remains inflamed and painful after all nonsurgical
treatments have been tried, your doctor may recommend surgical removal of the bursa. Removal of the bursa
does not hurt the hip, and the hip can function normally without it.
A newer technique that is gaining popularity is arthroscopic removal of the bursa. In this technique, the bursa
is removed through a small (1/4-inch) incision over the hip. A small camera, or arthroscope, is placed in a
second incision so the doctor can guide miniature surgical instruments and cut out the bursa. This surgery is
less invasive, and recovery is quicker and less painful.
Both types of surgeries are done on an outpatient (same-day) basis, so an overnight stay in the hospital is not
usually necessary. Early studies show arthroscopic removal of the bursa to be quite effective, but this is still
being studied.
Rehabilitation
Following surgery, a short rehabilitation period can be expected. Most patients find that using a cane or crutches for
a couple of days is helpful. It is reasonable to be up and walking around the evening after surgery. The soreness
from surgery usually goes away after a few days.
Prevention
Although hip bursitis cannot always be prevented, there are things you can do to prevent the inflammation from
getting worse.
Avoid repetitive activities that put stress on the hips.
Lose weight if you need to.
Get a properly fitting shoe insert for leg-length differences.
Maintain strength and flexibility of the hip muscles.
If you found this article helpful, you may also be interested in What Are NSAIDs? (topic.cfm?topic=A00284).
Last reviewed: March 2014
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an
educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should
consult his or her orthopaedic surgeon, or locate one in your area through the AAOS "Find an Orthopaedist" program on this website.
Copyright 2014 American Academy of Orthopaedic Surgeons
Related Articles
Bursitis de cadera (Hip Bursitis) (http://orthoinfo.aaos.org/topic.cfm?topic=A00724)
Hip Arthroscopy (http://orthoinfo.aaos.org/topic.cfm?topic=A00572)
How To Use Crutches, Canes, and Walkers (http://orthoinfo.aaos.org/topic.cfm?topic=A00181)
What Are NSAIDs? (http://orthoinfo.aaos.org/topic.cfm?topic=A00284)
Related Resources
Wellness: Hip Conditioning Program (/PDFs/Rehab_Hip_3.pdf)
OrthoInfo
The American Academy of Orthopaedic Surgeons
9400 West Higgins Road
Rosemont, IL 60018
Phone: 847.823.7186
Email: orthoinfo@aaos.org


